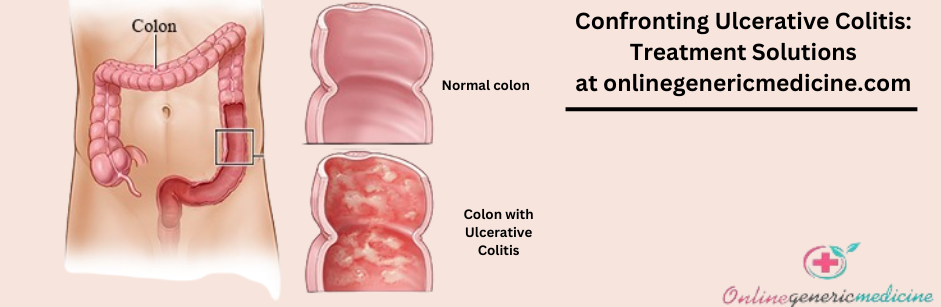
Ulcerative Colitis
-
-
-
-
-
Generic: MesalamineEquivalent Brand: Asacol30 Sachet/s$40.00
-
1. What is the main cause of colitis?
Symptoms
Ulcerative colitis symptoms can vary, counting on the severity of inflammation and where it occurs. Signs and symptoms may include:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- Rectal pain
- Rectal bleeding — demise bit of blood with stool
- Urgency to defecate
- Inability to defecate despite urgency
- Weight loss
- Fatigue
- Fever
- In children, failure to grow
- Most people with colitis have mild to moderate symptoms. The course of colitis may vary, with some people having a long duration of remission.
Types
Doctors often classify colitis as consistent with its location. Sorts of colitis include:
Ulcerative proctitis. Inflammation is confined to the world closest to the anus (rectum), and rectal bleeding could also be the sole sign of the disease.
Proctosigmoiditis. Inflammation involves the rectum and sigmoid flexure — the lower end of the colon. Signs and symptoms include bloody diarrhea, abdominal stiffness and pain, and impotence to maneuver the bowels in spite of the urge to try to do so (tenesmus).
Left-sided colitis. Inflammation continues from the rectum up through the sigmoid and colon. Signs and symptoms include bloody diarrhea, abdominal stiffness and pain on the left side, and urgency to defecate.
Pancolitis. This sort often affects the whole colon and sources bouts of bloody diarrhea which will be severe, abdominal cramps and pain, fatigue, and significant weight loss.
When to ascertain a doctor
See your doctor if you experience a persistent change in your bowel habits or if you've got signs and symptoms such as:
- Abdominal pain
- Blood in your stool
- Ongoing diarrhea that does not answer over-the-counter medications
- Diarrhea that awakens you from sleep
- An unexplained fever lasting quite each day or two
- Although colitis usually isn't fatal, it is a serious disease that, in some cases, may source life-threatening complications.
Causes
The exact explanation for colitis remains unknown. Then, diet and stress were suspected, but now doctors know that these factors may aggravate but don't cause colitis.
One possible cause is a system malfunction. When your system tries to repel an invading virus or bacterium, an abnormal immune reaction causes the system to attack the cells within the alimentary canal, too.
Heredity also seems to play a task therein colitis is more common in people that have relations with the disease. However, most people with colitis do not have this case history.
Risk factors
Ulcerative colitis affects about an equivalent number of girls and men. Risk factors may include:
Age. Colitis usually begins ahead of the age of 30. But it can occur at any age, and a few people might not develop the disease until after age 60.
Race or ethnicity. Although whites have the very best risk of the disease, it can occur in any race. If you're of Ashkenazi Jewish descent, your risk is alike higher.
Family history. You're at higher risk if you've got an in-depth relative, like a parent, sibling, or child, with the disease.
Complications
Possible complications of colitis include:
- Severe bleeding
- A hole within the colon (perforated colon)
- Severe dehydration
- Bone loss (osteoporosis)
- Inflammation of your skin, joints, and eyes
- An increased risk of carcinoma
- A rapidly swelling colon (toxic megacolon)
- Expanded risk of blood clots in veins and arteries
2. What foods trigger colitis?
Ulcerative colitis (UC) may have numerous triggers causing flare-ups and aggravation of the disease. Diet plays an important role in the patient’s overall health and quality of life. Diet is vital in maintaining healthy colon and gut bacteria. An appropriate diet can help in easy digestion, reducing tenderness, reducing complications, recovery from flare-ups, and recovery after surgery.
To increase the probabilities of remission, reduce digestive irritation and flare-ups, it's recommended that patients avoid or reduce the subsequent foods:
Whole-grain foods:
Foods that contain high fiber like whole-grain flour may trigger flare-ups. They are also harder to digest during a flare-up of UC, hence should be avoided.
Foods that consist of whole-grain flour are as follows:
- Cereals
- Whole grain bread, pasta, and noodles
- Brown rice
- Broken wheat or quinoa
- Oats
- Millets
- Barley
- Wheat berries
Seeds:
Seeds can provoke flare-ups and are difficult to digest. They contain insoluble fiber, which can cause bloating and diarrhea. Following seeds should be avoided:
- Millets
- Flax seeds
- Millet
- Sesame seeds
- Sunflower seeds
- Pine nuts
- Pumpkin seeds
Legumes:
- Legumes, including beans, lentils, soy, and peas, consist of high fiber and protein. They cause bloating and gas.
Nuts - Nuts, including nut-based flours and cheese, should be avoided because the high fiber in nuts are often difficult to digest. It’s usually advised to avoid the subsequent nuts:
- Hazelnuts
- Walnuts
- Almonds
- Peanuts
- Pecans
- Cashews
- Pistachios
- Almonds
Sulfate and sulfides:
- Sulfate may be a nutrient that assists in many body processes. However, in patients with UC, excess sulfates and sulfides within the diet may produce a toxic gas called sulfide causing bloating, abdominal pain, irritation, and foul-smelling gas.
Sulfate- and sulfide-rich food consumption should be decreased: - Red meat
- Dairy
- Beer and wine
- Apple and fruit juice
- Cruciferous vegetables
- Eggs
- Cheese
- Dried fruits
Fruits:
- Fruits contain high fiber that's difficult to digest. Fruits are often consumed if they need to be peeled, cooked, or as juice. Fruits should be avoided if they
- are raw,
- are canned,
- are dried and
- Contain seeds.
Vegetables:
Vegetables are a crucial source of nutrients in UC, but they also contain high fiber. Vegetables are often consumed if the skin has been peeled, and therefore the vegetables are cooked. Canned vegetables are often consumed. Pureed vegetables should be preferred because they're easy to digest.
Gluten:
- Gluten may be a protein found in wheat, rye, and barley. Gluten may be a common explanation for digestive intolerance causing gastric irritation. Gluten is found within the following food products:
- Bread
- Pasta
- Arranged products like condiments, sauces, soups, and proteins.
Dairy:
Intolerance to dairy products like milk, butter, yogurt, and cheese is common in patients with UC.








